With President-elect Donald Trump vowing to repeal and replace the Affordable Care Act, the law’s marketplace health coverage for uninsured individuals has never looked more vulnerable. What that means for Highmark and UPMC Health Plan — the only two remaining insurers offering marketplace plans in the Pittsburgh region — isn’t yet clear, but, then, the first few years of the program haven’t exactly been predictable.
For Highmark, it has meant crippling losses and a retreat from outlying counties, while UPMC Health Plan is now aggressively going after marketplace business in every Western Pennsylvania county and offering some of the lowest cost medium-range plans around.
Both insurers have been enrolling or renewing members since Nov. 1. Both say they are ready for the Jan. 1 start of the fourth cycle of the insurance marketplace — the centerpiece of a law that has made health insurance accessible for some 20 million Americans but that has also been marked by a balky launch of the healthcare.gov website, dropped plans, nail-biting Supreme Court rulings, shifting deadlines, a lopsided risk pool, higher than expected claims and rising premiums.
Many of the early problems may look like minor inconveniences compared with the threat the landmark legislation now faces. But they also may have set a course for its demise.
Early pricing strategies
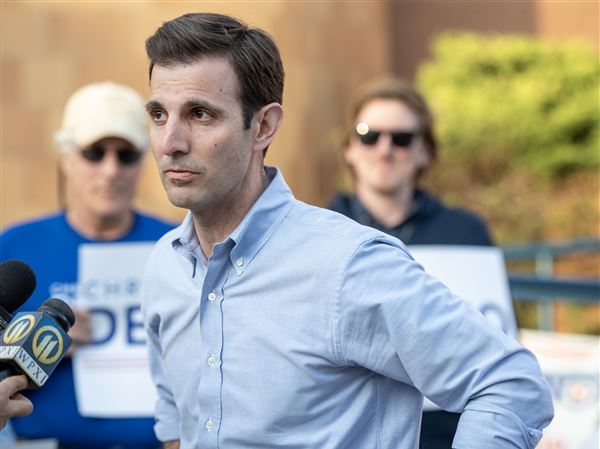
In autumn 2013, just weeks before the Affordable Care Act’s health insurance marketplace website would stumble out of the starting gate, Diane Holder, president and CEO of UPMC Health Plan, was reviewing rate numbers. She quickly realized the inaugural year would be a disappointment.
UPMC had spent two years planning for this, holding “meeting after meeting,” Ms. Holder said recently. Ultimately, the health plan offered 29 plans that first year — more than Highmark or any of the national insurers that had upped its presence in the Pittsburgh market in the wake of the Highmark-UPMC split.
UPMC’s actuaries had calculated plan premiums “to be competitive but not underpriced,” Ms. Holder said. For a mid-range ACA silver plan for a 40-year-old non-smoker, the monthly premium was $236.
A few blocks west, Highmark had moved aggressively price-wise into the marketplace, offering its silver plan for $163.19 per month. Highmark sold 99,000 plans in Western Pennsylvania alone that year.
UPMC Health Plan’s higher premiums proved less appealing, even though its rates fell in line with national insurers’ rates. For that first cycle, UPMC brought in about 4,500 new members, representing maybe 5 percent of the local market — a fraction of Highmark’s business.
Today, the picture looks much different.
Highmark has been hit with losses exceeding $800 million — $500 million of that from promised payments under the ACA’s “risk corridors” program, the insurer says.
The insurer had calculated the potential for other risks, too, but misjudged those risks. Enrollees — perhaps after years without coverage — swarmed to the health care system to address long-neglected, often chronic, medical issues. Meanwhile, young, healthy individuals whose premiums could have offset the cost of caring for the other group stayed out of the risk pool, undeterred by the threat of financial penalty.
By Highmark’s estimation, it was incurring $1.20 in costs for every $1 it took in revenue.
UPMC Health Plan’s slow start, meanwhile, turned out to be a blessing. With its limited risk pool exposure, its losses were much smaller, putting the insurer in a better position to adjust as the marketplace took hold.
Not that it was evident at the time. “We didn’t know if Highmark was going to make money or lose money,” said Ms. Holder, “and there wasn’t anybody in the country who could tell you because nobody knew.”
Now everyone knows and, with the fourth round of open enrollment underway through Jan. 31, the region’s major insurers have reversed marketplace roles in key respects. Highmark’s enrollment in the ACA marketplace, representing only a small percentage of its overall insurance book of business, stands at 48,300 in Western Pennsylvania, while UPMC covers 111,000.
For 2017, UPMC is offering plans in all 29 Western Pennsylvania counties and offers one of the lowest-cost mid-range silver plans in the U.S. Highmark has raised prices, while withdrawing from 17 of the 29 regional counties after finding the network structure in some counties financially unsustainable.
Highmark now plans to maintain a marketplace presence in only 12 of those counties: Allegheny, Beaver, Butler, Bedford, Blair, Cambria, Erie, McKean, Somerset, Venango, Washington and Westmoreland.
Younger, healthier, not participating
Roughly speaking, Highmark’s $800 million in marketplace losses can be attributed to two factors:
The first was a miscalculation about how much enrollees would use their newly acquired health coverage, even as younger, healthier people stayed away. The second was counting on early assurances by the Centers for Medicare and Medicaid Services that the federal government could cover insurers’ major marketplace losses through 2016.
“We didn’t know how people would react to the mandate [to buy insurance], whether it would be strong enough to get the younger, healthier risk group into the pool,” said Alexis Miller, Highmark’s senior vice president for its individual and small group business.
“We didn’t know that people would not pay premiums, that they could utilize the service and not pay the premium, only to return [to the marketplace] the following year.”
Highmark was far from alone in finding claim costs outpacing premium revenue, and Ms. Miller noted some other factors that came into play, such as rogue websites popping up across the Internet offering instructions on how to avoid paying for care.
The dearth of healthy folks heeding the individual mandate was “equally if not more critical” than the high use by those who did enroll, Ms. Miller said. “If the membership that moved into ACA would have been as risk diverse as was planned, I don’t think you would have seen the losses that we saw,” she said.
Then there was the now much-discussed issue of “risk corridors” payments, meant to protect insurers in the individual and small group markets against major claims costs during the first three years. Those are the same payments Highmark and a handful of others are now suing the federal government to collect.
The idea was simple: To help stabilize the marketplace in its early years, plans that profited above a certain amount would return some money to a pool, from which payments would be made to plans with higher-than-expected costs.
In an April 2014 bulletin, federal officials wrote, “We anticipate that risk corridors collections will be sufficient to pay for all risk corridor payments.”
But that sentence was immediately followed by this: “However, if risk corridor collections are insufficient to make risk corridors payments for a year, all risk corridor payments for that year will be reduced pro rata to the extent of any shortfall.”
Said Highmark’s Ms. Miller: “I would tell you that we paid more attention to the first part.”
Stephen Foreman, associate professor of health care administration at Robert Morris University, said CMS’ qualifying language boiled down to this: “If nobody made money, there wouldn’t be any money to shift to the ones that lost money.”
That’s how UPMC Health Plan interpreted it and the insurer set monthly premium prices that first year with no expectation that corridors payments would come their way. “We didn’t think there was anybody saving us if we bid too low,” said Ms. Holder.
Meanwhile, all across the country, participating insurers were making calculations and forecasts effectively blindfolded.
“If you think about how an insurance company looks at trends, you have to have some steady member participation,” Ms. Miller said. “You can’t look at the last two months and extrapolate for the next three years. Even going into the 2015 filing, we didn’t have a full set of consistent member performance that we could say, ‘This is a trend.’ ”
No payments coming
As for risk corridors payments, the first concrete sign of trouble from CMS didn’t come until October 2015, after insurers had already set out their plan offerings and had their rates approved for 2016. It was nothing short of a bombshell for Highmark:
For 2014, CMS said in the Oct. 1, 2015 bulletin, plans that had shown a profit would pay $362 million back to the risk corridors pool.
But, the agency said, those with unexpectedly high costs had submitted $2.87 billion in claims.
Only 12.6 percent of the insurers’ losses would be covered. For Highmark, that meant $500 million it had anticipated to cover its losses would not be coming.
That forced some recalibrating. “If the risk corridor is not going to help stabilize the market, then we need to turn to other things to consider,” Ms. Miller said.
In October, the Pennsylvania Insurance Department — concerned about insurers abandoning the marketplace — approved an average premium increase of 32.5 percent on individual plans.
The previous year, Ms. Miller noted, the department had approved a rate 26 percent below Highmark’s request; for 2017, the insurance department approved even higher rates than Highmark requested for some plans.
“Committed to this population”
UPMC Health Plan is moving ahead with its marketplace strategy. Ms. Holder said the health plan’s executives believe they can make those plans affordable and financially sustainable, starting with an underlying assumption that people who enroll will bear more similarity to Medicaid populations than to those commercially insured.
“We are used to a population that needs help and support,” Ms. Holder said. “We’re very committed to this population. We’re committed to staying in this business.”
UPMC Health Plan has experience with that demographic through various special programs dating back to 1996. “A lot of them didn’t have a traditional relationship with a physician,” she said. “They still weren’t used to using the system other than the emergency room.”
The insurer takes “a very, very aggressive” approach, making sure members see a primary care physician on a regular basis, offering gift cards arranging for transportation if necessary, and helping them manage chronic conditions, such as diabetes or high blood pressure.
President-elect Trump has signaled he would like to retain certain Affordable Care Act provisions, such as allowing children to stay on their parents’ plan to age 26 and protecting access to coverage for those with preexisting medical conditions.
His choice for incoming health and human services secretary, Georgia Rep. Tom Price, has offered his own replacement — the Empowering Patients First Act, which proposes age-adjusted tax credits for buying coverage and providing grants for states to set up high-risk pools. It does not include an individual mandate.
Whatever changes are coming, Ms. Holder said she would like to believe that “we live in a society where it’s important that people have access to care.”
“There has been a lot of good that has come out of the ACA, and I hope what happens is that they keep what’s good and fix the things that are bumpy.”
Steve Twedt: stwedt@post-gazette.com or 412-263-1963.
First Published: December 4, 2016, 5:09 a.m.