During the day, Ashley Benson guides patients through a busy pediatric ophthalmology office in Sewickley, scurrying from waiting room to patient room and back again.
But beginning in June 2022, her body began dictating a bathroom pit stop before greeting nearly every family, creating a daily tally of 10 or 15 bowel movements.
“I was so afraid,” Benson, of Evans City, said. “I didn’t want there to be an accident.”
At first, she thought maybe it was a case of food poisoning, since she had just been to a picnic. And she also wondered whether the symptoms were caused by the weight loss medication she started four months earlier, which already thinned her frame by 65 pounds.
Her symptoms were unignorable, but easy to explain away, especially for a healthy 32-year-old woman.
But she made a pact with herself: “If it persists, I’m calling my doctor.”
That decision likely saved her life.
A series of appointments and procedures later, Benson — a young wife and mother to a toddler — was diagnosed with stage I colon cancer.
Perhaps even more alarming, she’s far from alone.
While the overall incidence of colorectal cancer is decreasing, falling by an average of 1.8% each year from 2010 to 2019, cases of early onset CRC (or those in people under 50), have been climbing, by about 1.4% annually, with about 50% of those early onset cases occurring in people with no family history of the disease.
As a result, the U.S. Preventive Services Task Force lowered the recommended age for colon cancer screening in 2021 from age 50 to 45.
But that shift doesn’t protect patients such as Benson, which is why awareness created around this disease — spread, in part, by Colorectal Cancer Awareness Month each March — is vital.
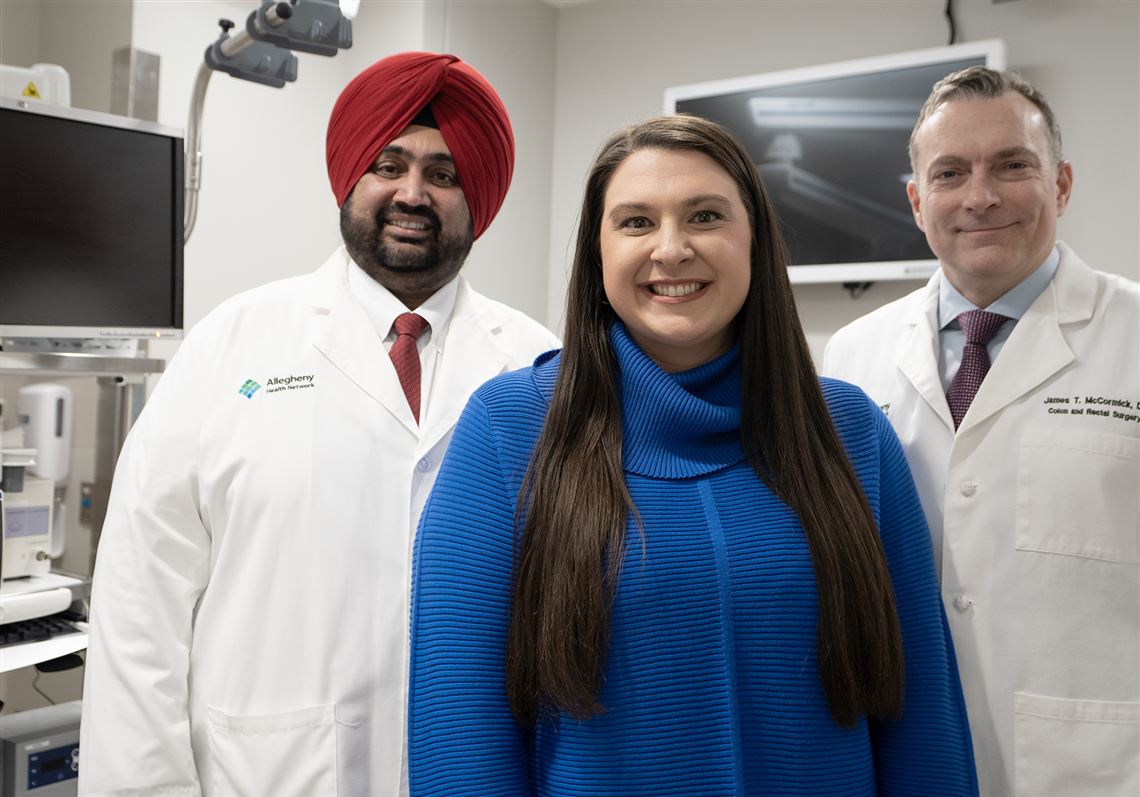
“Because there is no screening [guideline] to detect colon cancer for young people, we rely upon individuals to identify when something is abnormal,” James McCormick, chief of colon and rectal surgery for Allegheny Health Network, who treated Benson, said. “And then, rather than ignoring the symptoms or attributing them to something benign, doing something about it.”
Not only are there increases of CRC among the younger population, with evidence dating back to the mid-1990s for those ages 20 to 39, but increases in severity of those cases have also been observed.
This sounds alarm bells for medical professionals who view cancer trends among young adults as indicators of progress (or regress), as they reflect current threats to health rather than ones accumulated over a lifetime.
Gursimran Kochhar, AHN’s division chief of gastroenterology, who also treated Benson, explains that cause is multifactorial.
Some risk factors are unmodifiable, ones that cannot be changed, such as a genetic predisposition to CRC.
Those whose first-degree relatives (parents or siblings) have been afflicted with CRC have a different set of screening guidelines as a result, and should receive colonoscopies 10 years before that relative was diagnosed.
Other risk factors rely on choice.
“These modifiable risk factors are contributing in large part to these early onset cases of colorectal cancer,” Kochhar said. “Changes to the diet and the modern Western lifestyle is what we think is causing some of this.”
With evidence, he cites American obesity rates, lower intake of dietary fiber, increases in alcohol consumption and sedentary lifestyles among those potential causes.
The antidote, he said, is thinking about habits and diet in reference to “things our great grandparents did”: moving the body more, eating fresh foods rich in fiber, cooking at home, drinking water and finding ways to de-stress that doesn’t only involve watching TV, for example.
“I advise my patients not to make drastic changes,” he said. “Small changes that can be consistently maintained go a long way.”
Then, there’s how to react when GI symptoms arise.
Benson admits to the “oh, it’s nothing” approach for a short time. Now knowing the extent of her disease and required treatment, however, she can’t imagine what the outcome might have been had she not called her doctor.
One colonoscopy identified a 2½-inch precancerous polyp. Because of its irregular shape — flat and embedded in her colon wall rather than a finger-like protrusion — it took another colonoscopy and “bear claw” clip procedure to remove 80% of it. A follow-up colonoscopy, checking on the remaining 20%, revealed it was still growing, which is when Kochhar referred her to McCormick.
During her two-month path from clips to a bowel resection, the precancerous area in Benson’s colon turned cancerous, which she learned after about a foot of her colon and 28 lymph nodes were removed.
While rattling to hear accounts like Benson’s, ones that become more common with each passing year, it’s important to understand that they’re still relatively rare.
Prevalence data lags by about two to four years, but an article in CA: A Cancer Journal for Clinicians included a 2023 projection of 153,020 cases of CRC in Americans, with about 19,500 early onset cases and 3,750 resulting deaths.
Compare that to the total American population, approximately 333.29 million in 2022 and, in theory, that should calm anxious thoughts that might arise every time a younger person experiences a GI misfire.
But even more helpful is a guide for when to seek care.
“Right now, the main focus is seeing if we can get everyone to do their part by getting the screening,” Kochhar said. “The numbers aren’t where they should be.”
In 2021, 71.8% of adults aged 50 to 75 had received colonoscopies — procedures that require drinking a liquid meant to clear the bowels, followed by an outpatient hospital procedure, under sedation, that allows a camera to inspect the colon, or large intestine.
Alternatively, Cologuard, which tests stools for evidence of colon cancer, is available for those who are medically unable to undergo a colonoscopy.
For abdominal pains or changes in stool appearance or frequency, Kochhar recommends observing the pattern for no more than four to six weeks before seeking care.
For small amounts of blood in the toilet bowl or on toilet paper, causes are wide-ranging but typically benign — hemorrhoids, for example. Large amounts of blood, or blood from the rectum that does not accompany a bowel movement, constitute a medical emergency.
For anything in the middle, or if questions linger, Kochhar has advice: “My rule of thumb is if you have blood in or around the stool, and you have never discussed this with your physician, and you don’t have hemorrhoids, discuss it with your PCP.”
Nearly a year post-op and cancer-free, Benson continues to receive gold stars from her medical team, as she’s refocused her diet. She eats from her gardens, where she’s now intentionally growing foods known to have a high fiber content to feed healthy gut bacteria.
She’s keeping every scheduled appointment, including her one-year follow-up with McCormick in May, and is assisting in the fight for CRC awareness by sharing her story so no one with concerning GI symptoms assumes they’re “nothing.”
While she credits her medical team, especially Kochhar and McCormick, for saving her life, the doctors know their jobs aren’t possible without educated and courageous patients willing to say something when they see (or feel) something unusual.
“It’s important to remember that she saved her own life by getting the colonoscopy in the first place,” McCormick said. “She has no family history of colon cancer, and is too young for [scheduled] screening. So, by her paying attention to her symptoms and getting the right care at the right time by conscientious doctors, this was caught early, and that truly saved her life.”
Abby Mackey is a registered nurse, and can be reached at amackey@post-gazette.com and IG @abbymackeywrites.
First Published: March 1, 2024, 10:30 a.m.
Updated: March 1, 2024, 7:14 p.m.