When Derek Stipetich sees friends these days, some notice that he has lost weight and is using a leg brace. If they ask him what happened, he asks a question back: “Do you have time for a story?”
As COVID-19 started to rage through the Pittsburgh area late last fall, the Stipetich household in Cecil was no exception. In early November, Mr. Stipetich was told someone he had seen at a work event had tested positive; a few days later he heard the same thing from a guest at his daughter’s birthday party. Mr. Stipetich didn’t have any symptoms but decided to get tested.
When the test came back positive, he quarantined himself at home away from his wife, Jodie, and daughter Cheyenne and experienced some intestinal distress as his only symptom. By the time his quarantine period was over, he felt fine.
For Mr. Stipetich, 50, a lifelong fitness fanatic, weightlifter and bodybuilder, the only side effect was that he couldn’t lift quite as much. “Everything seemed normal except for whenever I was training, I couldn’t lift as hard or heavy as I used to — My strength had been zapped,” he said.
At a post-COVID-19 checkup in January, Mr. Stipetich’s lungs were clear and all of his bloodwork was perfect. “They were just like, ‘Sometimes it takes people a while to get your energy back after having COVID. It’s very normal,’” said his wife. “We just assumed that he was one of the people who would have a harder time on the recovery end.”
A midlife crisis? Stress?
In April, around Easter, Mr. Stipetich remembers catching a minor cold. In May, he started to have some trouble sleeping, occasionally waking up in the middle of the night feeling as if he was suffocating. He was starting to take naps during the day.
His wife was concerned. He had just closed down his own title insurance company and had switched jobs, coming off a long winter of lockdowns.
Was he depressed? Stressed? Having a midlife crisis from turning 50? At one point, she even told him he looked jaundiced, prompting ridicule from their daughter, who shares Mr. Stipetich’s olive skin tone from his Serbian and Croatian heritage. “It’s the color of our people,” Cheyenne shot back.
But after Mr. Stipetich started sleeping upright, wedged in a corner against the couch, Ms. Stipetich went online and found a primary care physician who could see him that day. On May 28, Mr. Stipetich worked from home and worked out in the morning, then drove to the noon appointment.
The doctor “took my blood pressure and took an [electrocardiogram] and said, ‘Who drove you here?’” said Mr. Stipetich. “I said, ‘Myself,’ and he said, ‘No, really, who drove you here?’ He looked me in the face and said, ‘You have [atrial fibrillation]. You have to go to the ER right now.’”
Life support
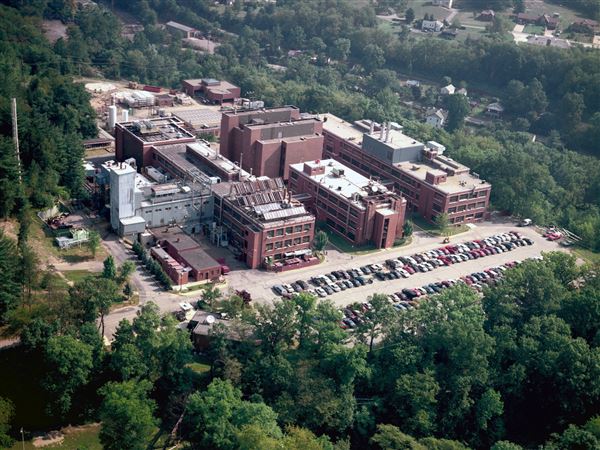
At Canonsburg Hospital, doctors ran tests and told Mr. Stipetich he needed to be transferred immediately to Allegheny General Hospital. Weather prevented a helicopter flight, so he was taken 25 miles by ambulance.
“The ambulance driver, I have to give her the utmost credit because she drove like she should be in NASCAR,” said Mr. Stipetich. “It seemed like it was right next door as fast as she got me there.”
By the time Ms. Stipetich and daughters Cheyenne, 14, and Sierra, 21, got to AGH, Mr. Stipetich was behind the doors of the cardiac catheterization lab.
When the doctors came out, it was to tell the family Mr. Stipetich was being placed on an ECMO machine, considered a form of life support. “By the time we saw him, he was in florid shock — the most extreme form of heart failure,” said Dr. Azam Hadi, attending cardiologist at AGH.
Derek’s kidneys and liver were shutting down, Ms. Stipetich was told, and his heart was only functioning at about 10%. The ECMO machine, a mechanical heart, would take over to try to give his body a chance at recovery.
“I tell everyone it was the hardest night of my life,” said Ms. Stipetich. “I’m standing here with my girls and my mom and Derek’s dad, like, ‘How did I get here?’”
Infecting the heart
Although they didn’t know it right away, doctors now believe the culprit in Derek’s decline was his COVID-19 infection almost six months before.
“Our working diagnosis is that he got infected with COVID, and it did infect the heart,” said Dr. Hadi. “It can just linger on and slowly weaken the heart over time.”
Likely because Mr. Stipetich was in such good health, his liver and kidneys bounced back quickly once he went on the ECMO machine, regaining 70% of their function within days. His heart was different.
If patients have to go on an ECMO machine, ideally they will only be on it for a few days, said Dr. Hadi. The longer that a patient is on it the higher the risk of complications.
Indeed, as a week passed, he began to have nosebleeds and other clotting issues. At one point, he called a nurse because he felt wetness, only for her to find the bed soaked in blood as his leg bled uncontrollably. "My leg was bleeding from where they cut my leg open to put the ECMO in,” said Mr. Stipetich.
Doctors ultimately determined that if Mr. Stipetich was going to get off the ECMO machine alive, he would need a transplant. “They came in and had a discussion where they told us they needed to get serious about the heart transplant, that there was no way to repair the heart,” said Mr. Stipetich. “Well, it was not really a discussion. There were no other options.”
A transplant
Just days later, on June 4, Ms. Stipetich posted on her Facebook page with news. “Tonight at 9:45 we will receive the most precious gift any family could ever give us, a beautiful, perfectly beating heart,” she wrote. It was only nine days after her husband had first gone to the doctor.
Mr. Stipetich was able to get a heart so quickly because he entered the hospital so sick, said Dr. Hadi, noting that ECMO patients are prioritized. He was also lucky to have the blood type AB positive, said his wife, meaning he was a “universal recipient” who could receive a heart from anyone regardless of blood type.
A case of COVID-19 resulting in a heart transplant is extremely rare, said Dr. Hadi, who believes Derek’s case is the first in the Pittsburgh area. UPMC has not done any heart transplants due to COVID-induced illnesses, said spokeswoman Andrea Kunicky, although the hospital system has done a lung transplant.
There are scattered reports nationally and internationally of similar cases, such as a previously healthy 31-year-old man in Illinois who received a heart transplant after having COVID-19, also after less than two weeks on the waiting list for the organ.
Dr. Hadi and his team analyzed Mr. Stipetich’s heart after it was removed and found signs consistent with a viral attack, which they presume to be from COVID-19.
“COVID can affect the heart,” said Dr. Hadi. “It can be inflammation caused by the virus itself that attacks the heart muscle and can lead to the heart becoming weak.”
Mr. Stipetich spent two weeks in the hospital recovering and getting educated on what life with his new heart would look like. He was back almost immediately to as much of a fitness regimen as he could muster, quizzing hospital staff on how the chicken was prepared and asking his wife to bring him Muscle Milk.
He is even weightlifting again, pleased that he was just able to front squat 100 pounds, even though it’s a far cry from the 1,200 pounds he was leg pressing in sets of eight last summer. He is not currently allowed to lift any weight involving his chest or back and only 5 pounds with his arms. As a side effect of his time on the ECMO machine, he developed a drop foot, unable to properly lift his toes. He is wearing a leg brace as part of his rehabilitation.
To ward off rejection of his new heart, he’s now taking 10 different medications each morning. His daughter Sierra, a ballet dancer and dance instructor who moved back home over the summer to help out, made a wooden sign for their porch telling guests an immunocompromised person lives there.
Pumping Adrenaline
The Stipetichs are starting a nonprofit, transitioned from Mr. Stipetich’s personal training business called Pumping Adrenaline, in hopes of helping others who find themselves navigating the heart transplant process with little notice.
Most other patients in the hospital had been on the transplant waiting list for years, their bodies extremely weak. Mr. Stipetich was awake and alert the entire time he was on the ECMO machine, even taking business calls and meetings.
“The transplant world for COVID patients is a lot different,” said Ms. Stipetich. “It just knocks you out. You don’t have time to find your feet.”
They also want to raise awareness of the importance of being aware of symptoms even after the acute phase of COVID-19 has passed.
“You get that first clearance and you think, ‘OK, I’m normal. Nothing is wrong with me,’” said Ms. Stipetich. “What gets overlooked a lot is the aftercare. If there’s any way our story could help stop this from happening to one single other person, we would yell it from the rooftop.”
Anya Sostek: asostek@post-gazette.com.
First Published: October 9, 2021, 2:33 p.m.