The resurgence of COVID-19 infections throughout large regions of the United States — including Allegheny County — has seen the median age of patients drop to 29, reflecting the trend of young people without masks flocking to restaurants, bars, parties and beaches as the economy reopened.
Now, despite the raging level of new infections here and elsewhere, that lower age and smaller percentage of COVID-19 deaths has nurtured some optimism that the worst of the pandemic may be over.
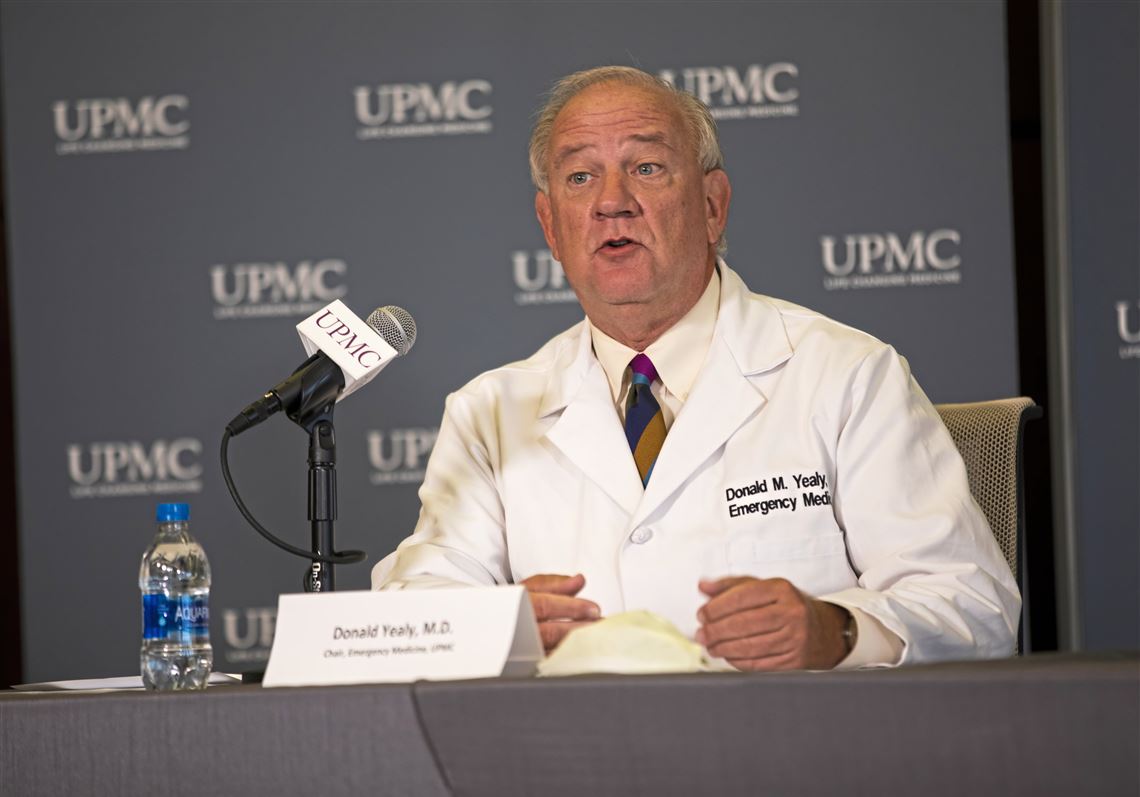
“We are not seeing the same pattern of severeness as we did before,” said Dr. Donald Yealy, UPMC senior medical director and chair of the Department of Emergency Medicine at UPMC and the University of Pittsburgh.
Contact tracing of UPMC patients has revealed that many younger patients had patronized bars or restaurants without wearing face masks while others returned from out-of-state vacations with the infection.
Among UPMC patients, only 2% of recent infections required hospitalization, with only one-tenth of those hospitalizations (.2% of all positive cases) resulting in death. Those results are due to various factors including the lower age of patients.
Dr. Yealy warned, however, that everyone should expect “the virus will be with us for the foreseeable future.”
Others are finding no good news in surging numbers of COVID-19 cases that have far exceeded those from early in the pandemic.
One chief concern is the many weeks of lag time between diagnoses and eventual health impacts — a situation that may be hiding the eventual impacts of the resurgence. It also raises potential for those who are asymptomatic to transmit the infection to the elderly and medically vulnerable.
An Allegheny Health Network infectious disease specialist said weeks of lag time that can extend to a month between infections, hospitalizations and even death means that it is way too soon to determine the full impact of record-high coronavirus cases.
“It is very troublesome seeing what we are seeing now,” said Dr. Tom Walsh, noting that AHN now has more COVID-19 hospitalizations than at any point during the pandemic. “We are seeing a lot of young, healthy people being hospitalized with serious infections and ending up on ventilation.
“We now are diagnosing people earlier in the disease than we were several months ago” due to availability of testing, with some people who are asymptomatic being confirmed to be infected.
As a result, the lag time is further extended, typically with two extra weeks for those who develop serious illness to require hospitalization, with another two or three weeks before death occurs.
And the idea — if you didn’t die from COVID-19, how bad can it be? — is rife with problems, he said.
“Eighty percent of this age group have mild disease,” he said. “But people hospitalized who don’t die can have long-term health problems — significant health problems — down the road due to blood clots and damage to the lungs. It can take a long time to return to normal.
“So no one is declaring victory after leaving the hospital with long-term complications.”
Evidence and strategy
Given past failures in predicting pandemic trends, many are now taking a wait-and-react approach.
UPMC data show “that we have been doing a good job in protecting those most vulnerable” to severe infection, including the elderly and those with preexisting conditions, said Dr. Graham Snyder, UPMC medical director of infection prevention and hospital epidemiology.
While more evidence is necessary, he said, UPMC more recently has been seeing a mutated SARS-CoV-2 strain that seems to be more infectious with higher viral loads but less virulence than the original strain that triggered the pandemic. That is supported by recent international studies about changes in the virus and its ability to mutate rapidly.
Another advance involves UPMC’s continual tweaking of its treatment therapies, given its involvement in various clinical trials, that physicians say is leading to fewer deaths and shorter hospital stays.
Dr. Snyder said UPMC has seen anecdotal benefits in using the anti-viral drug remdesivir, and the beneficial use of the corticosteroid drug dexamethasone to reduce the time people remain on ventilators.
In addition, convalescent plasma — blood plasma drawn from previously infected people that contains rich levels of antibodies against infection — also is showing positive treatment results.
UPMC physicians expressed support for the approach that Dr. Debra Bogen, executive director of the Allegheny County Health Department, is using to target problem zones, such as bars and restaurants, while allowing other segments of the economy to reopen.
But they, as with health officials nationwide, continue recommending that everyone continue wearing face masks in public, practice physical distancing along with occupancy limits for restaurants and public events.
Local trends
About a month ago, daily infections had dropped into single digits in Allegheny County but have escalated in recent weeks to triple digits, with three days in a row last week exceeding 200 newly diagnosed COVID-19 cases, along with 158 cases on Thursday and 180 cases on Friday. Those two days included 15 hospitalizations but only one death.
But there’s no evidence to date that the surge in positive COVID-19 cases throughout Western Pennsylvania, with 354 reported on Friday, will lead to the level of hospitalizations and deaths that occurred beginning in March, UPMC doctors said.
It also remains unclear whether reduced hospitalizations and deaths serve as a bellwether of pandemic decline or the calm before the storm of consequences from the new cases.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Disease, continued preaching not only caution but potential crisis during a recent interview with the JAMAlive — an online broadcast sponsored by the Journal of the American Medical Association.
“I hope these sobering numbers that we’re seeing are getting people to be jolted into realizing that not only do we have the responsibility to ourselves, we have societal responsibility to help put an end to this epidemic,” he said.
The two opposing forces, one focusing on public health and one focusing on opening the economy, are actually are seeking the same thing, he said.
The pandemic largely must be defeated before the bulk of the population ever feels comfortable about returning to a 2019 lifestyle.
“They’re not opposing the best way. The vehicle to reopening the country in a safe way is to prudently use public health measures,” Dr. Fauci said. “So it’s not public health against opening. It’s public health. They are complementary forces.”
Caution!
Dr. Amesh Adalja, an adjunct professor at Pitt’s School of Health and Rehabilitation Science now based at Johns Hopkins University, also is calling for caution, noting that people now contracting the virus tend to be younger and less likely to be hospitalized or die from COVID-19.
“But Arizona and Florida are seeing hospitalizations and deaths rising,” he said. “Deaths are a lagging indicator, and you only see results several weeks after diagnosis and that may rise weeks after cases increase and even longer.
“This is not a reason to relax. This is a different epidemiological picture with different cultures. The key is watching hospitalizations and make sure there is robust contact tracing.”
But as has been reported, contract tracing works best in keeping the pandemic at bay only when there is a low infection count. The resurgence in many areas that are keeping their economies open have put contract tracing operations “under water with resources and funding.”
“In many parts of the country, they can’t keep up with the number of cases,” Dr. Adalja said. “I hope they can get the help they need.”
During his recent interview, Dr. Fauci said he understands that young people may feel their risk of severe illness or death the virus is low.
“But remember,” he said, “there are many younger people who have underlying conditions that put them at risk of complications.”
“You’ve got to realize that even if you get infected and get no symptoms at all, you are propagating the pandemic dynamic,” he said. “The chances are you’re going to infect someone else who then will infect someone else, and then a vulnerable person will get infected.”
The numbers, the science and persistence of the pandemic continue to tell us so, he said.
David Templeton: dtempleton@post-gazette.com or 724-356-7535.
First Published: July 12, 2020, 10:00 a.m.